Today, the disease of arthrosis of the joints has become the most common among all pathologies of the musculoskeletal system. Moreover, urban dwellers, those accustomed to an inactive lifestyle and those who have recently suffered injuries of varying degrees of intensity, most often suffer from joint disorders.
Doctors' predictions in this regard are disappointing. It is assumed that in the near future the number of people suffering from various forms of arthrosis of the large joints will only increase. According to the latest data, about 7 percent have experienced all the symptoms and consequences of arthrosis.
This disease has become one of the leading causes of disability and decreased performance. It is characteristic that peak incidence occurs in the age group from 40 to 60 years, and not just older retirees, as is mistakenly believed.
What is arthrosis?
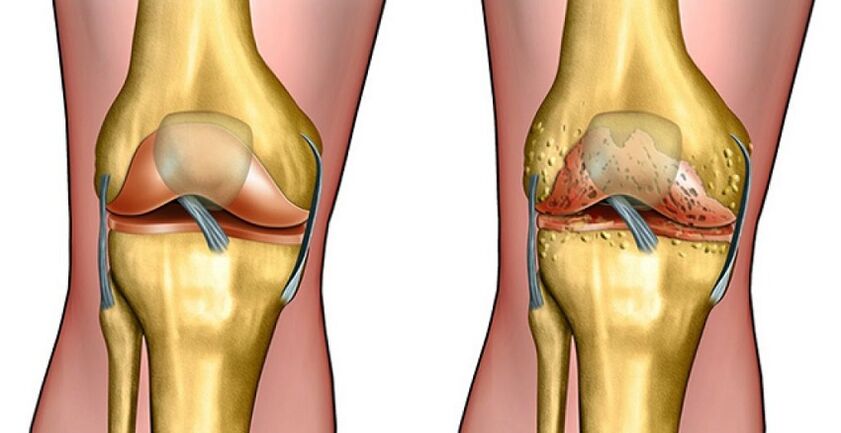
Arthrosis (another name for osteoarthritis) should be understood as a complex degenerative pathology in which the cartilage bone plates that make up the joint are destroyed. The reason is not just in the process that takes place in the hyaline cartilage.
There are many other conditions for this disease.
Arthrosis of the joints develops under the following conditions:
- excessive physical activity. Usually, overweight people get sick in such cases. Human joints are not designed for continuous movement with large loads. For this reason, the increased compression experienced by the knee during activity becomes a prerequisite for micro -trauma to cartilage tissue. There is a violation of the sliding properties of the tissue and a decrease in articular mobility. Athletes often suffer from systematic joint damage due to sharp and frequent changes in natural pressure between joint surfaces or high loads with unheated joints;
- congenital or acquired defects, injuries of the musculoskeletal system. In such cases, the disease is caused by insufficient contact of the articular surface of the bone. Absolutely the entire load cannot be channeled over the joint, and injuries are formed in places of excessive compression. Examples of such violations are rickets, scoliosis and kyphosis. It also includes improper consolidation of broken bones, various limb deformities;
- violation of cartilage regeneration. The mechanism of development of arthrosis is observed in the presence of inflammatory processes in the body, impaired blood circulation and hormonal disorders. The problem is based on inadequate cartilage tissue recovery, lack of natural regeneration and thinning;
- problems of synovial fluid formation and production. If the joint fluid is insufficient, the rubbing surface is constantly injured, its wear and inflammation increases rapidly, the general condition of the body worsens.
Stages of arthrosis
Since the disease of arthrosis provokes the destruction of cartilage tissue of the joints, its symptoms vary significantly depending on the stage of the pathological process.
As a result of active destruction of the joint surface, a person will experience new symptoms, and the prognosis for recovery of motor activity will not change. Based on the clinical picture of the disease, the doctor will select the optimal method of treatment and medication.
Grade 1 arthrosis is characterized by the fact that discomfort and slight pain are only felt after prolonged exercise. After a short rest, the symptoms that arise during physical activity fade.
In this case, the joint lesion will not be visible on X-ray photos, but there may be a slight narrowing of the joint space.
Stage 2 pathology is characterized by an increase in symptoms. Now there is pain not only as a result of prolonged activity, but also with small limb movements.
Rest will not bring the desired relief. There is stiffness in movement, limited joint movement. It is currently recommended to reduce the load on the affected joint, but should not be completely excluded, otherwise muscle atrophy will occur. X-rays will show clear signs of arthrosis:
- bone growth;
- change the shape;
- neoplasm (osteophyte) near the joint space, its narrowing.
When the disease reaches its final stages, lesions on the joints cause persistent pain. Thus, at the reflex level, a person begins to limit his movements sharply, to protect the affected joints from stress. Pain syndrome occurs even during sleep and rest, when the joints are at rest.
The patient is forced to assume the least painful position. Movement becomes possible only with the help of a wheelchair or cane.
It is characteristic that stage 3 and 4 arthrosis can completely eliminate a person’s ability to walk due to fusion of the articular surface (ankylosis).
Which joints are most often affected?
According to medical statistics, the lower part of the foot is most susceptible to arthrosis. Joints suffer from inflammation and degeneration: hips, knees.
If there is a problem in the hip joint, pain in the pelvis is initially felt after a long walk or run. With the active development of pathology, pain increases and mobility is limited.
One will notice an unpleasant stiffness in the joints, and at certain positions the stiffness increases several times at once. In the last stage of hip arthrosis, the patient consciously protects the affected foot and tries not to step on it at all. She did not move her pelvis, which helped relieve the pain.
Arthrosis of the knee joint is indicated by discomfort and pain after walking. There are no external manifestations of the problem and inflammation. The most common prerequisite for knee joint arthrosis is past trauma with a background of internal structural damage.
Such lesions, as a rule, cause abnormalities on the articular surfaces in contact. Also applies:
- overloading certain cartilage areas;
- their quick clothes.
The changes, as in previous cases, depend on the degree of arthrosis. You should also take into account the cause of the disease, the availability of adequate medical treatment, the general condition of the body and the dynamics of pathological processes. Some forms of the disease do not make themselves feel old and do not develop.
Sometimes, even for decades, there is no obvious deterioration in the knee. In other cases, there is a rapid increase in symptoms and a high probability of loss of mobility.
Eliminates arthrosis
Today, there are 2 main indications in the treatment of large joint arthrosis: medical and surgical.
First of all, treatment aims to improve blood circulation quickly in diseased joints and accelerate the properties of cartilage tissue with the help of medications. Anesthesia and elimination of inflammation are also required. For this purpose, doctors practice the use of the following drugs.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
This drug disrupts the natural chemical chains in cartilage that cause inflammation. There is swelling in the tissues, pain appears, and cartilage strength decreases during movement.
Thanks to the use of anti-inflammatory drugs, it is possible to reduce or completely stop the pain syndrome. The onset of the so -called chain inflammation process is also prevented, which helps accelerate the regrowth of the affected area.
The drug is produced in the form of tablets, powders and rectal suppositories. Treatment tactics, specific drug choices are determined by the doctor strictly individually, based on the clinical picture of the disease, its dynamics and corresponding pathology.
Opioids and chondroprotectors
Strong centralized pain relievers are called opioids. Usually, drugs like these have a narcotic effect on the body, increasing the level of pain sensitivity. Thanks to this treatment, pain in the affected joints can be reduced.
The use of drugs in this group should be under the supervision of the attending physician, as such drugs cause mental and physical dependence.
To accelerate the recovery of cartilage tissue, special methods are used - chondroprotectors. They are, in general, an element of the cartilage structure itself, which allows them to have an activating effect on its recovery.
These medications include:
- chondroitin sulfate;
- glucosamine sulfate;
- hyaluronic acid.
Chondroitin and glucosamine are organic substances that are abundant in the cartilage space. Their mechanism of action on the joints is not yet fully understood, however, has repeatedly been shown to have a positive effect on cartilage tissue regrowth during treatment.
Chondroitin-based drugs activate the production of special substances from the extracellular cartilage matrix (proteoglycans and hyaluronic acid). At the same time, the process of tissue reabsorption is significantly inhibited. In the same way, certain chemical processes are suppressed, there is a decrease in inflammation of the cartilage, damage and severity of the pain syndrome.
Long -term drug use in this group is often required. The course of treatment is required for at least 6 months. Otherwise, the benefits of therapy cannot be expected. An organic combination of chondroitin and glucosamine is more frequently practiced. However, clinical studies have not confirmed a significant difference between such treatment and the use of only one of the chondroprotectors.
While there are obvious benefits and safety, not everyone can treat joint arthrosis with such medications because of the high cost.
Hyaluronic acid is no less common in modern medicine. It is a long chain of carbohydrates that imparts elasticity and viscosity to synovial fluid. The unique properties of hyaluron are largely responsible for the good sliding properties of joint fluid.
Intra-articular injection of the drug has a beneficial effect on the condition of the body, as studies show that arthrosis is often triggered by a decrease in the concentration of hyaluron in the joint and the shortening of its molecular chain.



















